Health Behavior Models


Nasreen Hasan
November 30, 2023
You want to be healthy and you know what you need to do to be healthy. You know you should stop doom scrolling and go for a walk. But you don’t know how to make yourself do these things. Why not? Why is it so hard?
This is not a new concept. The Ancient Greeks had a word for this: Akrasia. Basically, Akrasia means doing the opposite of what you know is the best action. And the question as to why we do this has been debated since then to this very day. It could be that we prioritize other things. We want to eat healthy, but first we have to finish this task for work, and we can’t do that on an empty stomach, and it takes too long to cook a healthy meal. It could be that we get overwhelmed. We want to reduce our blood pressure, but there’s conflicting information about which foods to eat and which foods to avoid. It could be that we get discouraged too easily. We want to exercise, but after two or three sessions, we get tired and don’t see the results we hoped for, and decide it’s not worth it.
There are many reasons why it could happen. But what we need is to find a way to help us choose to do the right behavior. So, we are going to look at four different social science theories that can help us do just that
Health behaviors significantly influence our overall well-being. With various theories and models out there, understanding them helps us make sense of human behavior in relation to health and wellness. These models provide a framework for understanding how habits are formed and how they can be changed.
However it’s vital to understand that these models aren’t laws. They function within certain limits and assumptions, which may not always hold true across different contexts and individuals. They may overlook the uniqueness of personal experiences and socio-cultural backgrounds. Not everyone responds to health-related interventions in the same manner, and what works for one person may not work for another. Also, these models are typically based on the presumption that humans behave rationally, which is not always the case. Decisions about health behaviors can be influenced by emotions, stress, peer pressure and various other factors that may override rationality.
Therefore, while health behavior models provide valuable frameworks for understanding and influencing health behaviors, their limitations and assumptions must be acknowledged for a more realistic application.
Here, we will discuss some of these key models.
1. Health Belief Model (HBM)
The Health Belief Model posits that people take health-related action if they feel they can successfully avoid a negative health condition. It combines the person’s perception of the benefits of action and their self-efficacy.
Components of the Health Belief Model
The Health Belief Model further breaks down into several key components:
Perceived Susceptibility: This refers to an individual’s assessment of their risk of getting the condition.
Perceived Severity: This relates to a person’s belief about the seriousness of contracting an illness or of leaving it untreated. It includes considerations of medical complications and potential life disruptions.
Perceived Benefits: This relates to the belief in the efficacy of the advised action to reduce risk or seriousness of the impact.
Perceived Barriers: This involves the potential negative aspects of a health action that may act as impediments to undertaking the advised behavior.
Cues to Action: These are events, people, or things that prompt action. These cues can be internal (like body symptoms) or external (like media campaigns).
Self-Efficacy: This is the belief in one’s ability to successfully undertake the behavior required to achieve the desired outcome.
The Health Belief Model states that the root of these beliefs and perceptions come from demographic, social and psychological factors, and can be influenced by our level of knowledge.
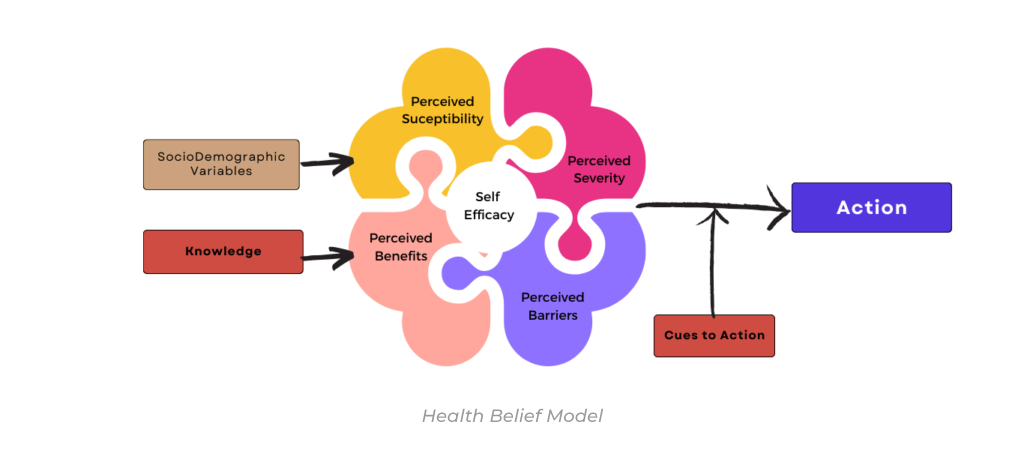
These components interact to influence health behavior, indicating that change is more likely if the individual believes they are susceptible to a serious health problem, and that change will result in a positive outcome.
Although all the elements of the Health Belief Model have the ability to motivate change, Perceived Barriers often emerges as the primary obstacle preventing individuals from adopting healthy behaviors. Common barriers include lack of time, financial constraints, age-related concerns and embarrassment. These barriers are often hard wired and therefore extremely difficult to overcome.
One effective method, and probably the easiest, for encouraging behavioral change is by manipulating “Cues to Action”. Cues to action serve as triggers that stimulate the decision-making process, leading to change in health behavior. These cues can be both internal (such as physical symptoms) and external (such as public health campaigns, advice from others, and mass media messages).
You can also Create Your Own Cues to Action. Here are some steps you can take:
1. Setting Reminders: These could be digital alarms on your phone or notes placed in areas where you spend most of your time. For example, a sticky note on your computer screen reminding you to take regular breaks for stretching can act as an effective cue.
2. Creating Visual Prompts: Visual cues like a pair of running shoes by the door or a water bottle on your desk can remind you to engage in physical activities or to stay hydrated throughout the day.
3. Leveraging Social Influence: Make use of social media or health apps that send reminders or health tips. A supportive social network can also provide external cues. For instance, a workout buddy can motivate you to stick to your fitness routine.
4. Using Personalized Affirmations: Regularly repeating affirmations that align with your desired health behavior can act as a mental cue, motivating you to make healthier choices.
5. Linking New Behaviors with Existing Habits: This involves creating a routine where a new behavior is associated with an existing one. For example, practicing meditation right after your morning coffee can create a strong cue for the new habit.
Remember, the effectiveness of cues to action can vary from person to person. It’s important to experiment and find what works best for you in your health behavior change journey.
2. Social Cognitive Theory (SCT)
The Social Cognitive Theory focuses on the idea of ‘reciprocal determinism’, where behavior, personal factors, and environmental influences all interact. It emphasizes that learning can occur by observing a behavior and the outcomes of that behavior.
Components of the Social Cognitive Theory
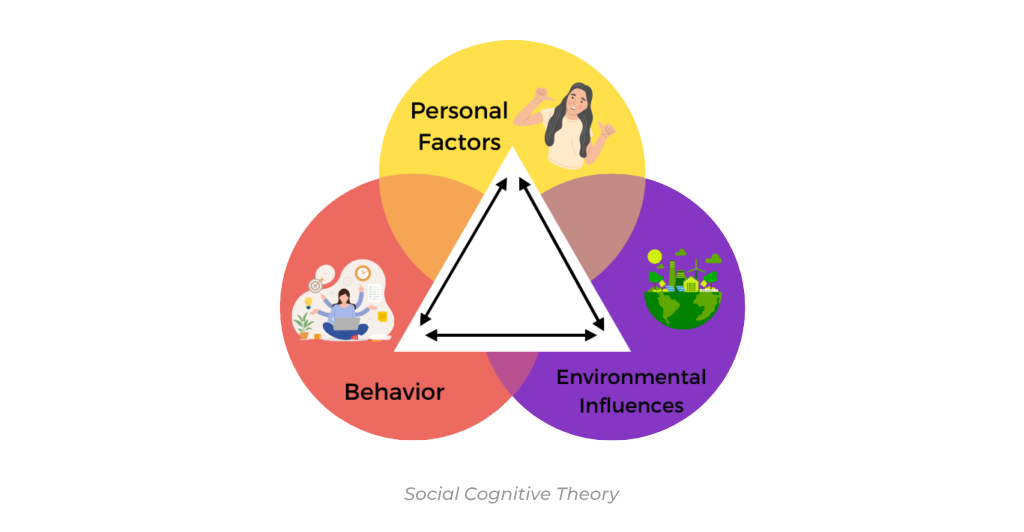
The Social Cognitive Theory (SCT) is built around several key components:
Observational Learning: This concept suggests that individuals can witness, comprehend, and replicate behavior just by watching others. It also implies that learning can occur without a change in behavior. The motivating factors include attention, retention, reproduction, and motivation.
Reinforcements: In SCT, reinforcements are responses to a person’s behavior that increase or decrease the likelihood of recurrence. These reinforcements can be self-initiated or from the external environment, and can be positive (increasing the likelihood of repeating the behavior) or negative (decreasing the likelihood of repeating the behavior).
Expectations: These are anticipated outcomes of a behavior. The decision to engage in a particular behavior is influenced by the expected results. This includes both outcome expectations (what a person expects will happen) and efficacy expectations (a person’s belief that they can successfully execute the action to produce the outcome).
Self-efficacy: This refers to an individual’s belief in their ability to bring about changes through their actions. Strong self-efficacy contributes to accomplishing tasks, overcoming difficulties, and maintaining behavioral changes.
Reciprocal Determinism: This denotes the dynamic interaction of the person, the behavior, and the environment in which the behavior is performed.
A central feature of SCT is the interplay of these components. The adoption, initiation, and maintenance of health behaviors are determined by these interacting factors. For instance, successful performance of a new behavior (like using a treadmill) can enhance self-efficacy, which in turn influences the person’s expectations and possibly their future behavior.
As such, SCT provides a comprehensive framework for understanding, predicting, and changing human behavior. It suggests that improving self-efficacy and outcome expectations, providing necessary skill sets, and establishing supportive environments are effective in promoting healthier behaviors. By understanding these components, we can develop more effective health promotion programs and interventions.
3. Transtheoretical Model (TTM)
The Transtheoretical Model emphasizes that behavior change is a process, not an event. It proposes that individuals move through different stages of change: precontemplation, contemplation, preparation, action, and maintenance.
Components of the Transtheoretical Model (TTM)
The Transtheoretical Model (TTM), also known as the “stages of change” model, approaches behavior change as a process that unfolds over time, involving progress through a series of stages.
Precontemplation: At this stage, individuals have no intention to change their behavior in the foreseeable future, often because they are unaware of their problematic behavior or they are demoralized after previous failed attempts to change.
Contemplation: Individuals acknowledge that they have a problem and begin to think about the possibility of change. However, they might also have ambivalence towards the change and remain in this stage for a long time.
Preparation: People at this stage plan to take action in the immediate future, usually measured as the next month. Typically, they have already taken some significant actions towards behavior change in the past year.
Action: The action stage is characterized by specific, noticeable modifications in a person’s behavior, experiences, or environment in order to overcome their problems.
Maintenance: In this stage, individuals work to prevent relapse and consolidate the gains attained during the action stage. This stage extends from six months to an indeterminate period past the initial action.
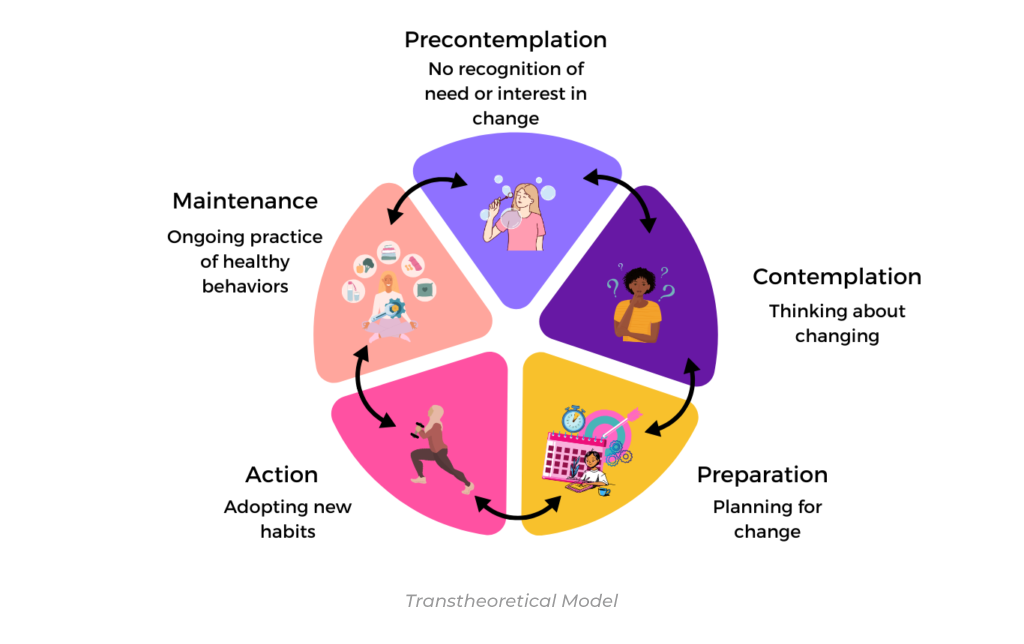
Moreover, TTM recognizes that individuals may experience relapses and recycle through the stages. This understanding underscores the complexity of sustained behavior change and the need for interventions to be adaptable and flexible to the individual’s stage. It is a powerful model that provides valuable insights into the complexity of health behavior change, aiding in the development of effective strategies for individual and population health improvement.
4. Social Ecological Model (SEM)
The Social Ecological Model is a comprehensive theoretical framework that takes into consideration the complex interplay of factors affecting health behaviors. It posits that health behaviors are not only determined by individual beliefs and attitudes, but also by the broader social, community, and societal contexts.
Components of the Social Ecological Model
The Social Ecological Model (SEM) comprises multiple levels of influence:
Individual: This level includes characteristics of the individual such as knowledge, attitudes, behavior, self-concept, skills, etc. It suggests that understanding individual-level factors is crucial in promoting health behaviors.
Interpersonal: This level explores the influence of interpersonal and social networks including families, friends, and peers. It emphasizes the role these relationships play in shaping behavior through mechanisms of support, social identity, and role modeling.
Organizational: This level examines the social institutions with rules and regulations for operations that can affect how, where, and when health behavior occurs. This includes workplaces, schools, and churches.
Community: This level looks into relationships among organizations, institutions, and informational networks within defined boundaries. This includes housing, community centers, and neighborhoods. This level focuses on national, state, and local laws and regulations that impact health behaviors either directly through control or indirectly through influencing other levels of the SEM.

Each of these levels interact with one another, and changes at any level will in turn influence the other levels. By incorporating all these levels, the SEM provides a more holistic perspective of health behavior, highlighting the multifaceted and interactive effects of personal and environmental factors. It illustrates the importance of interventions targeting multiple levels of influence to achieve substantial and lasting health behavior change.
Which Model is Best?
Choosing the appropriate behavioral model is largely contingent on our individual characteristics and the circumstances surrounding the desired behavior change. It is crucial to understand the stage of change, self-efficacy, and our personal, social, and environmental influences.
Through an understanding of these models, we can develop effective strategies to promote healthier lifestyles and achieve behavior change. Additionally, by recognizing that behavior is a complex process that unfolds over time in multiple contexts, we can create interventions tailored to our individual needs for maximum effectiveness. With this knowledge, we can begin to make progress towards our goals of achieving improved health outcomes through behavior change.
References: Social and Behavioral Theories – OBSSR

